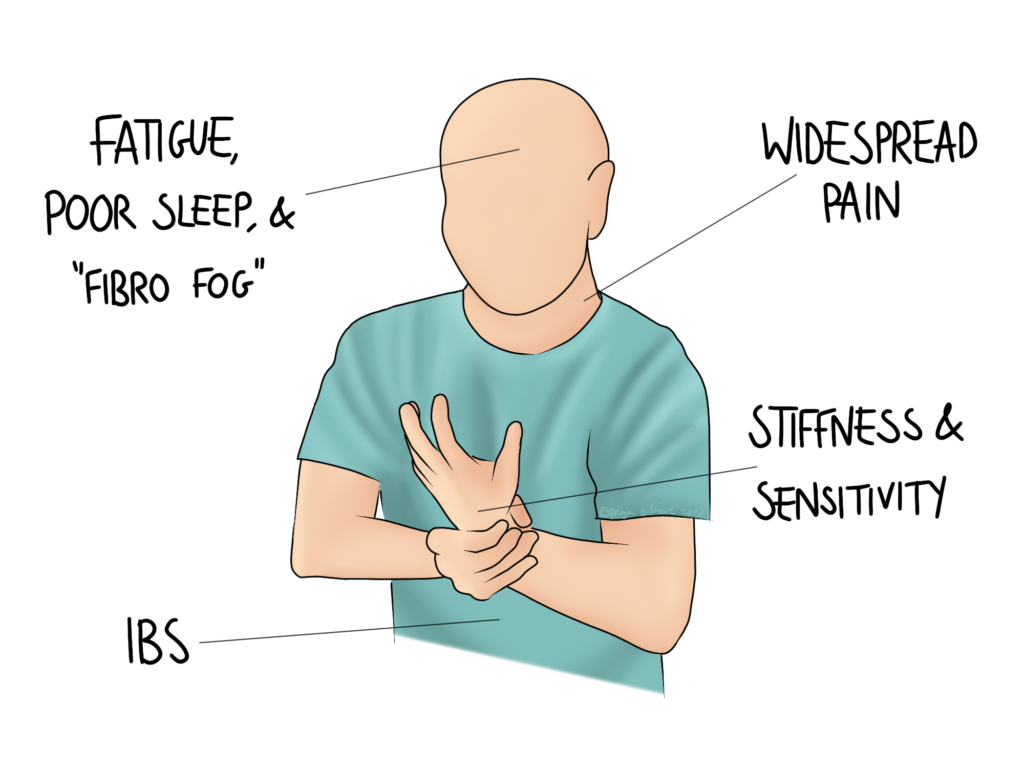
Both the public and medical profession continue to understand more about fibromyalgia as time goes on, but it is still a long way from being fully understood. The condition causes a range of symptoms, including pain, cognitive changes, fatigue, and IBS-type symptoms. Although there is no one test for it, there is a detailed diagnostic criteria, and if you suffer from it, it’s not “all in your head”.
What is Fibromyalgia?
Fibromyalgia is considered a rheumatological condition, affecting women more than men. Figures vary dramatically, but the ratio may be as extreme as 4 women to every 1 man diagnosed with the condition. However, diagnosis can be slow and difficult, so numbers of diagnosed cases may not be truly reflective of the real numbers of people suffering.
The cause (or causes) of the condition are unclear, but generally accepted to be a combination of factors. They may include:
- A genetic predisposition
- An association with another condition, such as ankylosing spondylitis
- Changes to the way the nervous system signals
Like some autoimmune conditions, the onset of fibromyalgia often follows a trauma, whether emotional, like a bereavement, or physical, like an injury or giving birth. It has been theorised that an infection, like a virus, could also be a potential trigger.
With this in mind, it makes sense that the condition is categorised as “functional”. IBS is an example of another functional condition: all this means is that investigations will not show a structural issue (whereas something like Crohn’s disease would). This might make diagnosis a bit more difficult, but there are still tools to hand for a rheumatologist to label the condition.
Diagnosis
Diagnosing fibromyalgia addresses three aspects of the symptoms:
- widespread pain
- severe pain
- other body symptoms, such as fatigue, weakness, headaches, and IBS
Blood tests and scans can be useful to rule out other conditions, but they won’t show fibromyalgia as such. Other painful conditions that present with similarities, like rheumatoid arthritis, are likely to show on these tests. The absence of their signs would help your doctor to form a treatment plan, and make a diagnosis of fibromyalgia more likely.
Diagnosis is primarily done through a questionnaire, a copy of which can be found here. As mentioned above, it requires widespread, severe pain, and other somatic symptoms. These symptoms need to present for at least 3 consecutive months.
Osteopathy and Fibromyalgia
The best thing someone can do to help manage their symptoms is to increase their exercise. When you’re fatigued and in pain, exercise feels like an unnatural choice, but it’s not something you need to jump straight into. Your osteopath can help you to improve your comfortable movements through work to the joints and muscles. With this increased capacity, you might find that you can now manage a 10 minute daily walk. And when you can manage the short walk, maybe you’ll be able to push yourself to do two, or to extend the first.
We can help to support you as you increase your exercise, providing specific activities to try, and working on your aches and pains as they change. Some people prefer to start with very gentle treatment- in these cases, cranial osteopathy may be the best place to start. We can always modify treatment as we progress, so let us know if that’s what you’d like when you make your appointment.
Make an appointment for your fibromyalgia with Beverley here
